BLOG: NEWS, RECIPES AND ARTICLES
Oatmeal Protein Snack Cookies
Packed with oats for sustained energy, creamy almond butter for healthy fats, and a boost of protein powder, these cookies are a nutritional powerhouse disguised as a treat.
The Power-Packed Oatmeal Cookie: A Healthier Grab-and-Go Option for Busy Families
As a functional medicine physician and natural food chef, I'm always on the lookout for nutritious alternatives to processed snacks.
Let's face it – in the rush of busy mornings or between activities, it's easy to reach for commercially available granola bars. While convenient, these often come loaded with unwanted ingredients, excess sugars, and artificial additives that don't align with our health goals.
That's why I developed this oatmeal cookie recipe with a twist. Packed with oats for sustained energy, creamy almond butter for healthy fats, and a boost of protein powder, these cookies are a nutritional powerhouse disguised as a treat.
Oatmeal Protein Snack Cookies
Author: Erica Leazenby, MD
Yields: 12 cookies
Time: 35 minutes
Ingredients:
2 cup whole oats (gluten free if needed)
1/2 cup almond flour
1 scoop collagen powder
1 serving unsweetened, unflavored plant-based protein powder (I use So Lean & So Clean brand)
1/2 tsp backing powder
1/2 tsp baking soda
1/2 tsp cinnamon
1/4 tsp sea salt
2 large eggs
1/2 cup natural almond butter
1/2 cup maple syrup
1/4 cup olive oil or coconut oil
1 tsp vanilla
1/2 cup dark chocolate chips
1/3 cup walnut or pecan pieces
Directions:
Preheat oven to 350 (325 convection). Line a baking sheet with parchment paper.
Combine the oats, almond flour, collagen, protein powder, baking powder, baking soda, cinnamon and salt in a mixing bowl. Stir until well mixed.
In a separate bowl combine the eggs, almond butter, maple syrup, oil and vanilla until well mixed.
Mix the wet and dry ingredients until a thick batter is formed. Add the walnuts/pecan and chocolate chips and stir again to evenly distribute.
Divide the batter into 12 equal serving on the prepared baking sheet. Bake for 22-28 minutes or until the cookies are golden brown. Allow them to cool before removing from the sheet. Store in an air tight contain. These cookies freeze well.
Nutrient estimate: 303 kcal, total fat: 19.7g, Carb: 26.2g, Fiber 4.3g, Protein 9.8g
Small Healthy Habits For The New Year
As December 2024 draws to a close, it’s the perfect time to pause and reflect on the journey we’ve taken this year.
As December 2024 draws to a close, it’s the perfect time to pause and reflect on the journey we’ve taken this year. With the hustle and bustle of the holiday season, many of us may find ourselves looking back at our resolutions and goals, considering what we’ve accomplished and what we still aspire to achieve. Whether you’ve made strides in your health journey, embraced new habits, or faced challenges along the way, remember that every step contributes to your growth. As we prepare to welcome a new year, let’s take a moment to celebrate our progress and set our intentions for 2025. This is not just about resolutions; it’s about cultivating a mindset that embraces continuous improvement and well-being. Join me as we explore ways to reflect on the past year and create a roadmap for a healthier, more fulfilling future!
Putting small healthy habits into practice with more frequency helps take the pressure off maintaining a year-long streak. Consider these smaller goals:
Try a month-long challenge like a Dry January (or Feb, March or April) or a Whole30 elimination diet. Researchers found that participants of a Dry January maintained a “significant reduction” in their alcohol consumption six to eight months later. A month-long challenge to your eating and drinking habits can pay health dividends long into the future.
Try a weekly screen-free Sunday. Reclaiming a few hours from your phone or computer can improve your physical health, boost your mood, and free up time for play and community.
Try a daily routine like morning mindfulness or evening gratitude journaling. Mindfulness allows us to understand our emotions better, potentially helping us feel calmer. Research shows that gratitude can support better health, happiness and wisdom in ourselves and our community.
If your 2025 goals include getting hormones back in balance, addressing pesky stubborn weight, finally figuring out your gut symptoms or optimizing your labs for longevity, I’m here for you. At Relish Health we work together to help you reach your goals and best health.
Relish Health Gift Guide 2024
It’s that time of year again when we think about how to show our love to family, friends and community.
Happy Holidays from our home to yours! The season of gift-giving is officially here, and few things are sweeter to me than finding the perfect gifts for loved ones - gifts that make them feel known and loved. I’ve pulled together some of my favorite health-enhancing gift ideas, and hope this guide gives inspiration, relieves shopping frenzy, and enables you and your loved ones to savor the season.
Consider some of these options:
For the women in your life:
Hormone health has been a trending topic this year. (It’s about time we demistify this important topic.) There are several great books to gift:
For the traveler:
Exercise is foundational to health and longevity. These items help me stay active while I’m away from home and the gym:
For the foodie:
Celebrate the season with mocktails. I love to mix shrubs and bitters with sparkling water for festive alternative to the traditional cocktail.
The Gift for You:
ProLon is a fasting mimicking diet system that gives you all the benefits of a 5-day fast while enjoying food. Increased focus, fat focused weight loss, enhanced cellular renewal and improved metabolic health are well documented benefits. (Learn more about the fast here.) Prolon kits can be purchased through Fullscripts or pick up at the Relish Health office.
A food focused reset with a LIVE, PHYSICIAN GUIDED 50-DAY PROTOCOL TO UNCOVER FOOD INTOLERANCES, HEAL YOUR GUT & REGAIN YOUR HEALTH
Some gifts never go out of style. Check out the gift guides from
2018, 2019, 2020, 2021, 2022, and 2023
(This blog post is not sponsored by any manufacturer. However, at no cost to you, Relish Health may receive a commission on purchases made through an Amazon link.)
The Intricate Dance of Gut Microbes and Hormones: A Key to Women's Health
Our bodies are home to trillions of microorganisms, collectively known as the microbiome. Recent research has shed light on the fascinating relationship between the gut microbiome and our hormonal systems, particularly in women. This interplay has far-reaching implications for various aspects of health, from reproductive issues to metabolic disorders.
Our bodies are home to trillions of microorganisms, collectively known as the microbiome. Recent research has shed light on the fascinating relationship between the gut microbiome and our hormonal systems, particularly in women. This interplay has far-reaching implications for various aspects of health, from reproductive issues to metabolic disorders.
The Gut Microbiome: More Than Just Digestion
The gut microbiome is a complex ecosystem of bacteria residing in our intestines. Far from being passive inhabitants, these microbes play crucial roles in our overall health. They influence not only digestion but also our immune system, metabolism, and even our mood. Remarkably, the gut microbiome is now considered an endocrine organ in its own right, capable of producing and regulating hormones.
Estrogen and the Gut: A Two-Way Street
One of the most significant interactions occurs between gut bacteria and estrogen, a primary female sex hormone. This relationship is so important that researchers have coined the term "estrobolome" to describe the collection of gut bacteria capable of metabolizing estrogen. Here's how it works:
Some gut bacteria produce an enzyme called β-glucuronidase, which helps activate estrogen in the body.
An imbalance in these bacteria can lead to either too much or too little active estrogen, potentially contributing to conditions like endometriosis, PCOS, and certain cancers.
Conversely, estrogen itself can influence the composition of the gut microbiome, creating a feedback loop.
Androgens and Gut Health
While often considered male hormones, androgens like testosterone also play crucial roles in women's health. Elevated androgen levels, a condition known as hyperandrogenaemia, are common in PCOS and can affect the gut microbiome. Studies have shown that:
High androgen levels correlate with changes in specific gut bacteria populations.
These alterations may contribute to the metabolic issues often seen in PCOS, such as insulin resistance and obesity.
Implications for Women's Health
Understanding these intricate relationships opens up new avenues for addressing women's health issues:
Personalized Medicine: By analyzing an individual's gut microbiome, healthcare providers might better predict and treat hormonal imbalances.
Novel Treatments: Probiotics or targeted dietary interventions could potentially help manage conditions like PCOS by modulating the gut microbiome.
Preventive Care: Maintaining a healthy gut microbiome through diet and lifestyle choices may help prevent hormonal issues before they arise.
Fertility Support: For women struggling with fertility, addressing gut health could be a complementary approach to traditional treatments.
Conclusion
The discovery of the gut microbiome's role in hormonal health is revolutionizing our understanding of women's health. It underscores the importance of a holistic approach to healthcare, considering the interconnectedness of various bodily systems. While research in this field is still evolving, it's clear that nurturing our gut health through a balanced diet, regular exercise, and stress management could have far-reaching benefits for hormonal balance and overall well-being. As we continue to unravel the mysteries of the gut microbiome, we may find new keys to addressing long-standing health challenges, offering hope for more effective and personalized treatments in women's health.
Steps to Prepare You for Bioidentical Hormones
References:
Qi X, Yun C, Pang Y, Qiao J. The impact of the gut microbiota on the reproductive and metabolic endocrine system. Gut Microbes. 2021 Jan-Dec;13(1):1-21. doi: 10.1080/19490976.2021.1894070. PMID: 33722164; PMCID: PMC7971312.
He S, Li H, Yu Z, Zhang F, Liang S, Liu H, Chen H, Lü M. The Gut Microbiome and Sex Hormone-Related Diseases. Front Microbiol. 2021 Sep 28;12:711137. doi: 10.3389/fmicb.2021.711137. PMID: 34650525; PMCID: PMC8506209.
Navigating the Mental Health Maze of Perimenopause: A Functional Medicine Perspective
As a functional medicine physician, I've witnessed countless women struggle with the often-overlooked mental health challenges of perimenopause. This transitional phase, typically occurring in your 40s or early 50s, is more than just hot flashes and irregular periods. It's a complex interplay of hormonal shifts, life changes, and biological processes that can significantly impact your mental well-being. In this post, we'll dive deep into the vulnerability of mental health during perimenopause, exploring why it happens, how it manifests, and most importantly, what you can do about it. Whether you're in the thick of perimenopause or approaching this life stage, understanding these changes can empower you to navigate this transition with greater ease and resilience.
As a functional medicine physician, I've witnessed countless women struggle with the often-overlooked mental health challenges of perimenopause. This transitional phase, typically occurring in your 40s or early 50s, is more than just hot flashes and irregular periods. It's a complex interplay of hormonal shifts, life changes, and biological processes that can significantly impact your mental well-being. In this post, we'll dive deep into the vulnerability of mental health during perimenopause, exploring why it happens, how it manifests, and most importantly, what you can do about it. Whether you're in the thick of perimenopause or approaching this life stage, understanding these changes can empower you to navigate this transition with greater ease and resilience.
The Perimenopausal Landscape: More Than Just Physical Changes
Perimenopause, the period leading up to menopause, is often misunderstood. While many women are prepared for the physical symptoms, the mental and emotional shifts can catch them off guard. Let's break down why this phase of life can be particularly challenging for mental health.
Hormonal Havoc: The Root of the Issue
At the heart of perimenopausal changes lies a dramatic shift in hormonal balance. Estrogen and progesterone, two key players in women's health, begin to fluctuate wildly during this time. These hormones don't just affect your reproductive system; they play crucial roles in brain function and mood regulation. Estrogen, in particular, has a significant impact on neurotransmitters like serotonin, often called the "feel-good" chemical and GABA. As estrogen levels become erratic and eventually decline, it can lead to:
Mood swings
Increased irritability
Higher risk of depression and anxiety
In my practice, I've seen how these hormonal changes can make women feel like they're on an emotional rollercoaster. One patient described it as "feeling like a stranger in my own skin."
The Sleep-Mood Connection
One of the most underappreciated aspects of perimenopause is its impact on sleep. Night sweats, insomnia, and disrupted sleep patterns are common complaints. But what many don't realize is how profoundly this can affect mental health. Poor sleep quality can increase the risk of depression up to tenfold. It's a vicious cycle: hormonal changes disrupt sleep, poor sleep exacerbates mood issues, and mood issues can further impact sleep quality. Breaking this cycle is often key to improving overall well-being during perimenopause.
Cognitive Changes: The "Brain Fog" Phenomenon
Many of my patients express frustration with cognitive changes during perimenopause. They often describe:
Difficulty concentrating
Problems with short-term memory
Reduced mental clarity, often referred to as "brain fog"
These cognitive shifts can be particularly distressing for high-achieving women who have always prided themselves on their mental acuity. It's important to understand that these changes are real and rooted in the hormonal shifts occurring in your body.
Life Transitions: Adding Fuel to the Fire
Perimenopause often coincides with a period of significant life changes. Many women find themselves juggling multiple roles and facing new challenges:
Caring for aging parents
Navigating changes in relationships as children leave home
Career transitions or increased work responsibilities
Personal health concerns
These external stressors can compound the internal hormonal changes, creating a perfect storm for mental health vulnerabilities. It's no wonder that many women feel overwhelmed during this time.
The Hidden Epidemic: Depression and Anxiety in Perimenopause
Research indicates that the risk of experiencing depressive symptoms during perimenopause can be as high as 40%. This is a staggering number, yet many women suffer in silence, unaware that their symptoms are related to this life transition. Anxiety, too, is a common companion during perimenopause. Many women report feeling more worried, experiencing panic attacks, or developing new phobias during this time. These mental health challenges can be particularly confusing for women who have never experienced them before.
A Functional Medicine Approach to Perimenopausal Mental Health
As a functional medicine practitioner, I believe in addressing the root causes of health issues rather than just treating symptoms. When it comes to perimenopausal mental health, this means taking a comprehensive approach that considers all aspects of a woman's life and health.
1. Comprehensive Hormone Testing
Standard hormone tests often miss the nuances of perimenopausal hormone fluctuations. In my practice, I use more comprehensive hormone panels that look at:
Estrogen and its metabolites
Progesterone
Testosterone
Cortisol patterns throughout the day
Thyroid function
This detailed analysis helps us understand the unique hormonal landscape of each woman, allowing for more targeted interventions.
2. Addressing Nutrient Deficiencies
Nutrient deficiencies can exacerbate perimenopausal symptoms. I often test for and address deficiencies in:
Vitamin D
B vitamins, especially B12 and folate
Magnesium
Omega-3 fatty acids
These nutrients play crucial roles in mood regulation, energy production, and overall brain health.
3. Gut Health Optimization
The gut-brain connection is powerful, and optimizing gut health can have profound effects on mental well-being. I focus on:
Identifying and addressing food sensitivities
Balancing the gut microbiome
Healing gut permeability ("leaky gut")
Many of my patients are surprised to learn how much their digestive health impacts their mood and cognitive function.
4. Lifestyle Modifications
Lifestyle changes can be incredibly powerful in managing perimenopausal symptoms:
Regular exercise, especially strength training and yoga
Stress reduction techniques like meditation or mindfulness practices
Prioritizing sleep hygiene
Nutrition focused on anti-inflammatory, whole foods and adequate protein intake
These changes not only help with symptom management but also support overall health and longevity.
5. Targeted Supplementation
While I always prefer to address nutrient needs through diet, targeted supplementation can be beneficial during perimenopause. Some supplements I often recommend include:
Adaptogens like Rhodiola or Ashwagandha for stress management
Omega-3 fatty acids for brain health and mood stabilization
Magnesium for sleep and mood support
Herbal remedies like DIM, Black Cohosh or Maca root for hormone balance
It's crucial to work with a healthcare provider to determine the right supplements for your individual needs, as what works for one woman may not be appropriate for another.
6. Bioidentical Hormone Therapy
For some women, bioidentical hormone therapy can be a game-changer. Unlike synthetic hormones, bioidentical hormones are chemically identical to those your body produces naturally. This therapy can help:
Stabilize mood swings
Improve sleep quality
Enhance cognitive function
However, hormone therapy isn't right for everyone. It's a decision that should be made carefully, considering your individual health history and risk factors. I recommend seeking the help from a physician that is a certified menopause expert by the North American Menopause Society.
7. Mind-Body Techniques
The power of mind-body techniques in managing perimenopausal symptoms shouldn't be underestimated. I often recommend:
Cognitive Behavioral Therapy (CBT) for managing anxiety and depression
Mindfulness-Based Stress Reduction (MBSR)
Yoga or Tai Chi for stress relief and hormonal balance
These practices can help you develop resilience and coping strategies that extend far beyond managing perimenopausal symptoms.
The Importance of Community and Support
One aspect of perimenopausal mental health that often gets overlooked is the importance of community and support. Many women feel isolated during this transition, unsure of where to turn for help or understanding. I encourage my patients to:
Join support groups or online communities for perimenopausal women
Have open conversations with friends and family about their experiences
Seek out mentors who have successfully navigated this life stage
Remember, you're not alone in this journey. Sharing your experiences and learning from others can be incredibly empowering and healing.
A Word on Seeking Professional Help
While lifestyle changes and natural interventions can be incredibly effective, it's important to recognize when professional help is needed. If you're experiencing persistent feelings of depression, anxiety, or other mental health concerns, don't hesitate to seek help from a mental health professional. There's no shame in needing extra support during this transitional time. In fact, seeking help is a sign of strength and self-awareness.
Embracing the Transition: A New Perspective on Perimenopause
As we wrap up this exploration of mental health in perimenopause, I want to offer a shift in perspective. While this phase of life certainly comes with its challenges, it also offers opportunities for growth, self-discovery, and empowerment. Many women emerge from perimenopause with:
A deeper understanding of their bodies and health
Increased self-awareness and emotional intelligence
A renewed sense of purpose and direction in life
By addressing the mental health aspects of perimenopause head-on, you're not just managing symptoms – you're setting the stage for a vibrant, healthy, and fulfilling next chapter of your life.
Conclusion: Your Perimenopausal Journey
Navigating the mental health challenges of perimenopause can feel overwhelming, but remember – you have more control than you might think. By understanding the underlying causes of these changes, adopting a holistic approach to your health, and seeking support when needed, you can not only survive but thrive during this transition. As a functional medicine practitioner, I'm passionate about empowering women to take charge of their health during perimenopause and beyond. This phase of life doesn't have to be a struggle. With the right knowledge, support, and strategies, it can be a time of profound personal growth and renewed vitality. Remember, your perimenopausal journey is unique to you. Honor your experiences, listen to your body, and don't hesitate to seek the support and care you deserve. Here's to embracing this transition with confidence, grace, and optimism for the exciting journey ahead!
References:
Jagtap BL, Prasad BS, Chaudhury S. Psychiatric morbidity in perimenopausal women. Ind Psychiatry J. 2016 Jan-Jun;25(1):86-92. doi: 10.4103/0972-6748.196056. PMID: 28163413; PMCID: PMC5248425.
Behrman S, Crockett C. Severe mental illness and the perimenopause. BJPsych Bulletin. Published online 2023:1-7. doi:10.1192/bjb.2023.89
Alblooshi S, Taylor M, Gill N. Does menopause elevate the risk for developing depression and anxiety? Results from a systematic review. Australas Psychiatry. 2023 Apr;31(2):165-173. doi: 10.1177/10398562231165439. Epub 2023 Mar 24. PMID: 36961547; PMCID: PMC10088347.
Menopause: Understanding the Fundamentals
Menopause is a natural biological process that marks the end of a woman's reproductive years. It's a significant transition that every woman experiences, typically in her late 40s or early 50s that occurs over several years. Let's delve into the fundamentals of menopause, exploring its definition, the hormones involved, and the symptoms that women may experience.
Menopause is a natural biological process that marks the end of a woman's reproductive years. It's a significant transition that every woman experiences, typically in her late 40s or early 50s that occurs over several years. Let's delve into the fundamentals of menopause, exploring its definition, the hormones involved, and the symptoms that women may experience.
What is Menopause?
Menopause is officially defined as the point when a woman has gone 12 consecutive months without a menstrual period. It signals the end of fertility and the cessation of ovarian function. The average age of menopause in the United States is 51 years, though it can commonly occur anywhere between the ages of 45 and 56. It's important to note that menopause itself is not a condition that needs treatment. Rather, it's the symptoms and increased health risks associated with the hormonal changes of menopause that may require management.
The Stages of Menopause
The menopausal transition is often divided into three stages:
Perimenopause: This is the transitional phase leading up to menopause. It typically begins in a woman's 40s but can start in the 30s. During this time, the ovaries gradually produce less estrogen and progesterone, and menstrual cycles may become irregular. Other symptoms can include mood changes, changes in sexual desire, trouble concentrating or with memory, increasing headaches, night sweats or hot flashes, vaginal dryness, trouble with sleep, joint and muscle aches, heavy sweating, urinary frequency, and PMS.
Menopause: This is the point at which a woman has had her final menstrual period, confirmed after 12 months without a period.
Postmenopause: This refers to the years following menopause. During this time, menopausal symptoms may ease for many women, but the health risks related to the loss of estrogen increase.
Hormones Involved in Menopause
The primary hormones involved in menopause are:
Estrogen: This is the main female sex hormone. It plays a crucial role in regulating the menstrual cycle, supporting pregnancy, and maintaining bone density, among other functions. During perimenopause estrogen levels can fluctuate widely. Once menopause occurs, estrogen levels are consistently low.
Progesterone: This hormone prepares the uterus for pregnancy and regulates the menstrual cycle. Its production also decreases during menopause. Early symptoms in perimenopause are often caused by low progesterone.
Follicle-Stimulating Hormone (FSH): As estrogen levels drop, the body produces more FSH in an attempt to stimulate the ovaries. High FSH levels are often used as an indicator of menopause.
Luteinizing Hormone (LH): Like FSH, LH levels increase as the body tries to stimulate ovarian function.
Testosterone: While primarily thought of as a male hormone, women also produce small amounts of testosterone. Its levels may decrease during menopause, potentially affecting libido and energy levels.
Early Symptoms of Menopause
As women enter perimenopause, they may start experiencing various symptoms due to hormonal fluctuations. These early symptoms can include:
Irregular Periods: This is often the first sign of approaching menopause. Menstrual cycles may become longer or shorter, heavier or lighter.
Vasomotor Symptoms (aka Hot Flashes and Night Sweats): About 75% of women experience hot flashes, which are sudden feelings of heat that spread over the body, often accompanied by sweating and flushing, but some women may also experience chills. In early perimenopause, symptoms often start as night sweats around the time of a women’s period. As the perimenopause transition progresses, flushing may occur day and night all month long.
Mood Changes: Some women may experience mood swings, irritability, or increased risk of depression.
Vaginal Dryness: Decreasing estrogen levels can lead to vaginal dryness, which may cause discomfort during intercourse.
Sleep Disturbances: Many women report difficulty falling asleep or staying asleep, often due to night sweats.
Changes in Libido: Some women may experience a decrease in sex drive.
Weight Gain and Slowed Metabolism: The hormonal changes of menopause can make it easier to gain weight and harder to lose it. This can increase the risk of type 2 diabetes.
Late Symptoms of Menopause
As women progress through menopause and into postmenopause, they may experience additional symptoms:
Bone Loss: The decrease in estrogen leads to accelerated bone loss, increasing the risk of osteoporosis and fractures.
Cardiovascular Changes: The risk of heart disease increases after menopause, partly due to the loss of estrogen's protective effects on the cardiovascular system.
Urinary Issues: The decrease in estrogen can lead to thinning of the vaginal and urethral tissues, potentially causing urinary incontinence and increased risk of urinary tract infections.
Skin Changes: The skin may become drier and less elastic due to decreased collagen production.
Hair Changes: Decreased collagen production can lead to thinner, drier skin and changes in hair texture and growth patterns. Some women may notice thinning of hair on the scalp and increased facial hair growth.
Mood and Cognitive Changes: Some women report difficulties with memory and concentration, often referred to as "brain fog". Research in this area is ongoing. Menopause increases vulnerability to depression and anxiety, perhaps via estrogen fluctuations affecting serotonin and GABA.
Managing Menopausal Symptoms
While menopause is a natural process, its symptoms can be disruptive to daily life. There are several approaches to managing these symptoms and reducing the risks associated with low estrogen:
Lifestyle Changes: Regular exercise, a balanced diet, stress reduction techniques, and avoiding triggers (like spicy foods or alcohol for hot flashes) can help manage symptoms.
Hormone Therapy: For many women, hormone therapy can be an effective treatment for menopausal symptoms. While not suitable for everyone, there are significant benefits to hormone replacement therapy. The risks of treatment are low, but should be discussed with a menopause-trained, healthcare provider.
Non-Hormonal Medications: There are various non-hormonal medications that can help with specific symptoms, such as antidepressants for mood changes or osteoporosis medications for bone health.
Alternative Therapies: Some women find relief through alternative therapies like acupuncture or herbal supplements, although scientific evidence for their effectiveness is often limited.
The Future of Menopause Research
As our understanding of menopause continues to evolve, research is ongoing in several areas:
Personalized Medicine: Researchers are working on ways to predict the onset and severity of menopausal symptoms based on genetic and other individual factors.
Novel Treatments: New non-hormonal treatments for menopausal symptoms are being developed and tested.
Long-term Health Effects: Studies are exploring the long-term health implications of menopause and how to best protect women's health in the post-menopausal years.
Quality of Life: There's increasing focus on understanding and improving quality of life for women during and after the menopausal transition.
Conclusion
Menopause is a natural and inevitable part of every woman's life. While it can bring challenges, it's also an opportunity for women to take charge of their health and well-being. Understanding the fundamentals of menopause - from the hormonal changes to the range of potential symptoms - can empower women to navigate this transition more effectively. It's crucial to remember that every woman's experience of menopause is unique. What works for one woman may not work for another. Open communication with healthcare providers, partners, and other supportive individuals can make a significant difference in managing this transition. As research continues to advance our understanding of menopause, women have more options than ever for managing symptoms and maintaining their health. By staying informed and proactive, women can approach menopause not as an ending, but as a new chapter in their lives - one that can be filled with health, vitality, and new opportunities for growth and self-discovery.
Relish Health is here to help you navigate your menopause transition.
References:
Alblooshi S, Taylor M, Gill N. Does menopause elevate the risk for developing depression and anxiety? Results from a systematic review. Australas Psychiatry. 2023 Apr;31(2):165-173. doi: 10.1177/10398562231165439. Epub 2023 Mar 24. PMID: 36961547; PMCID: PMC10088347.
Erdélyi A, Pálfi E, Tűű L, Nas K, Szűcs Z, Török M, Jakab A, Várbíró S. The Importance of Nutrition in Menopause and Perimenopause-A Review. Nutrients. 2023 Dec 21;16(1):27. doi: 10.3390/nu16010027. PMID: 38201856; PMCID: PMC10780928.
Introduction to Menopause; John Hopkins Medicine. Accessed 8/31/24.
Office of Women’s Health; US U.S. Department of Health & Human Services Accessed 8/31/2024
Peacock K, Carlson K, Ketvertis KM. Menopause. [Updated 2023 Dec 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
Menopause 101: A primer for the perimenopausal; North American Menopause Society. Accessed 8/31/2024
Guilliams, T., Supporting the Menopausal Transition. The Standard Monograph Series. Vol 20, No. 1. 2024.
Steps to Prepare You for Bioidentical Hormones
The symptoms and changes that occur in perimenopause and menopause are natural, however, women now have access to bioidentical hormones that can help alleviate symptoms such as hot flashes, insomnia, and mood swings. Additionally, many individuals opt for hormones for their benefits to the health of the brain, bones, heart, as well as preventing dryness and atrophy in skin and vaginal tissues.
Consider these steps to prepare for hormone therapy:
The symptoms and changes that occur in perimenopause and menopause are natural, however bioidentical hormones that can help alleviate symptoms such as hot flashes, insomnia, and mood swings. Additionally, many individuals opt for hormones for their benefits to the health of the brain, bones, heart, as well as preventing dryness and atrophy in skin and vaginal tissues.
Bioidentical hormones are demonstrated to be safe when prescribed appropriately by a physician who comprehensively understands your medical history and appropriately monitors your dosage. Despite their low-risk nature, it's essential to recognize that they are not entirely without risks. Therefore, if opting for hormone therapy, seek guidance from a knowledgeable prescriber who conducts in-person physical examinations, uses bioidentical products, and follows the steps outlined below.
5 Steps to prepare you for hormone replacement therapy:
Boost your own hormone production to reduce reliance on prescriptions. You still produce hormones in menopause, just in smaller quantities. Your sex hormones—estrogen, progesterone, and testosterone—are crafted from cholesterol in your cell's mitochondria. So, optimizing cholesterol and ensuring healthy mitochondrial function is crucial. Check your cholesterol levels with a fasting lipid test and consider evaluating your mitochondrial health by checking targeted nutrient levels or oxidative stress markers.
Enhance your hormone signaling for optimal production. Messenger chemicals from your brain, specifically the hypothalamus and pituitary glands, play a crucial role in signaling hormone production. However, this communication system can falter when your sleep, exercise, or stress levels are out of balance, leading to disrupted cortisol. A comprehensive plan for hormone replacement includes stratagies to optimize these important lifestyle habits.
Revitalize your hormone receptors to address low hormone symptoms. Often, the issue isn't just insufficient hormone production or inadequate replacement hormone intake; it's the malfunctioning of receptors. The culprits behind receptor dysfunction is often inflammation. Inflammatory cytokines can clog up hormone receptors, preventing your precious hormones from attaching. This scenario is particularly evident in cases of insulin resistance.
Here's a two-fold approach to tackle inflammation:
Investigate potential sources of inflammation, including dysregulated blood sugar (either too low or too high), obesity, heightened stress, sleep apnea, anemia, allergies, inflammatory foods, gut dysbiosis, and chronic infections.
Adopt an anti-inflammatory diet. Focus on eating lots of veggies and adequate protein— whole foods that are minimally processed. Ensure your intake of EPA and DHA omega-3 fats is sufficient. These fats help reduce inflammation. You can check your omega-3 levels with an Omega Check at Quest or Labcorp to determine your omega-3 levels and supplement accordingly. Remember, the dose on a fish oil bottle might not be the right fit for your individual needs.
Ensure efficient breakdown and elimination of hormones. Your liver and gut play vital roles in managing your hormones. Hormones go through two phases of liver processing and are then expels into your GI tract through bile, where beneficial gut bacteria further break them down before they are excreted. Efficient hormone breakdown is crucial to prevent the backup or reabsorption of estrogen metabolites. Some women may face challenges in hormone metabolism due to genetic factors, fatty liver, or alcohol use. Before starting any hormone regimen, even topical hormones, ensure you're experiencing healthy bowel movements daily. Taking proactive steps in hormone breakdown and elimination contributes to overall well-being.
Reduce your exposure to endocrine disruptors. These are chemicals pervasive in our environment that function as xenoestrogens. Xenoestrogens are “foreign” estrogens, substances that are close enough in molecular structure to estrogen that they can bind to estrogen receptor sites with potentially hazardous outcomes. Sources of xenoestrogens include plastics, pesticides, chemicals, and water systems. To limit exposure, prioritize organic foods, opt for clean beauty and household products, steer clear of hair dye and nail polish, and strictly avoid consuming or drinking from any plastic containers. Heat exacerbates the issue, so be particularly cautious with items like water bottles left in the car.
If you’d like to learn more about avoiding endocrine disruptors, explore the guides provided by the Environmental Working Group for valuable insights and tips. Taking these steps empowers you to minimize exposure and support a healthier endocrine system.
Want some help determining if hormones are right for you? Scheduled an appointment with Relish Health.
A Functional Medicine and Obesity Specialist’s Approach to Weight Loss
In functional medicine, we approach weight loss much differently than the conventional world. Oftentimes, when the root cause of a condition are addressed, weight loss naturally occurs.
A functional medicine approach to weight management includes:
I have exciting news-- I completed an Obesity Medicine Fellowship through Columbia University Institute of Human Nutrition, accredited by the American Board of Obesity Medicine in 2023. Learning is my superpower, passion, and hobby. With Ozempic’s (semaglutide) new popularity, I want to make sure you are getting access to the most up-to-date weight management treatments with expert level care.
In functional medicine, we approach weight loss much differently than the conventional world. For starters, we believe it is important to note that your weight is NOT the cause of your symptoms. Weight bias in healthcare is a real issue, and unfortunately many clinicians are quick to blame excess weight as a cause of illness rather than digging deep into a health issue to treat the condition holistically. Oftentimes, when the root cause of a condition are addressed, weight loss naturally occurs.
Through my educational journey this past year I learned best practices for prescribing all types of weight loss medications. I am so grateful to have medications in my “toolbox” to support you. Sometime they are the necessary and previously missing ingredient for weight loss success. When appropriately used, these medications complement the whole-body, functional medicine approach to health that may ultimately promote weight loss.
A functional medicine approach to weight management includes:
Reducing Inflammation. Inflammation is one of the first factors we address in a functional medicine weight loss approach. Inflammation is your body’s way of fighting against infection and injuries in an attempt to heal itself. Over time, certain factors may cause low-grade, chronic inflammation that is detrimental to your weight loss efforts. Stress, toxins, gut infections, food sensitivities, and poor nutrition can all play a role in causing low-grade inflammation. Through personalized testing, I aim to identify potential causes of inflammation to tailor the best treatment plan for you.
Insulin resistance occurs when your cells become resistant to insulin, a hormone responsible for controlling blood sugar levels. If you have insulin resistance, you may experience frequent sugar cravings, fatigue after meals, weight gain or difficulty losing weight, and constant hunger. Your diet is the best way to reverse insulin resistance. However, rather than focusing on restriction or a trendy diet, I want to help you identify your macronutrient needs and a lifestyle eating pattern that you can follow for the long run.
Optimizing your gut health is important. Your gut plays a crucial role in your overall health and weight loss efforts. More specifically, beneficial gut bacteria help you maintain a healthy gut lining, prevent overgrowth of harmful bacteria, and may even regulate your metabolism. Having a healthy and diverse balance of gut bacteria may prevent weight gain over time.
Assess your hormones. All our hormones work together like a beautiful symphony. Optimizing thyroid health and sex hormones can play a role in maintaining weight. Hypothyroidism affects nearly 12 percent of all Americans and may cause unintentional weight gain or hinder weight loss efforts.
Support Natural Detoxification. Your body has a system in place to eliminate toxins and waste products. However, a typical American lifestyle usually entails a high toxic load with a nutrient-deficient diet. Unfortunately, this pairing may cause disruptions in your natural detox mechanisms. During functional medicine weight loss, we aim to support detoxification by 1) supporting the body with nutrient rich food that supports liver health, 2) increasing intake of antioxidants, and 3) optimizing pathways in which your body can eliminates toxins via sweat, urine, and bowel movements.
Weight loss is not as simple as the diet industry may want you to believe. A functional medicine approach identifies and treats the root causes of your symptoms and can promote weight loss in the process.
At Relish Health I support a mindset of abundance versus restriction. Rather than focusing on the scale, we can help you identify and treat various factors that may ultimately promote sustainable weight loss.
Dark Chocolate Pot de Cream with Fresh Raspberries
This recipe is a little gem. It is so decadent and delicious yet lacks gluten, dairy and excessive sugar. The ingredients come together quickly. Using a blender is a cheater’s way to make sure your custard is smooth and silky rather than lumpy.
This recipe is a little gem. It is so decadent and delicious yet lacks gluten, dairy and excessive sugar. Even better the ingredients come together quickly. Using a blender is a cheater’s way to make sure your custard is smooth and silky rather than lumpy.
Dark Chocolate Pot de Crème with Fresh Raspberries
Yields: 6 servings
Time: 15 minutes active time, 2+ hours resting time
Ingredients:
1 13.5 ounce can full-fat coconut milk
2 eggs
2 Tablespoons maple syrup
1 teaspoon vanilla extract
Pinch sea salt
5 oz. dark chocolate chips (about 1 cup chips)
Fresh raspberries (or another berry)
Optional additional garnish: Coconut whipped cream and chocolate shavings
Directions:
Wisk together the coconut milk, eggs, maple syrup, vanilla and salt in a medium saucepan. Gently warm the mixture until it is steaming and starting to coat the back of a spatula. Do not let the mixture boil.
Place the chocolate chips in the blender. Once the coconut milk mixture is steaming and starting to thicken, pour it into the blender over the chocolate. Purée the chocolate and coconut mixture until it is smooth, and the chocolate is fully melted.
Pour the chocolate cream into 6 ramekins. Gently tap the ramekins to release air bubbles from the cream.
Chill for the pot de cream to allow it to solidify. The cream will be a pudding-like consistency in about 1-2 hours. Refrigerate longer for a firmer mousse-like consistency.
Remove the pot de cream from the refrigerator about 10 minutes before serving to allow them to come to room temperature. Garnish with fresh raspberries.
The Ultimate Blood Sugar Test: Understanding your A1c
At Relish Health, a hemoglobin A1c (HbA1c or A1c) is a routine lab. It measures the extent to which hemoglobin in the blood has been affected (“glycosylated’) by blood sugar. Optimizing blood sugar balance is important for controlling inflammation and promoting longevity. With over 100 million Americans living with diabetes or pre-diabetes and millions more with suboptimal blood sugar balance, having a clear picture of your blood sugar levels is crucial.
At Relish Health, a hemoglobin A1c (HbA1c or A1c) is a routine lab. It measures the extent to which hemoglobin in the blood has been affected (“glycosylated”) by blood sugar. Optimizing blood sugar balance is important for controlling inflammation and promoting longevity. With over 100 million Americans living with diabetes or pre-diabetes and millions more with suboptimal blood sugar balance, having a clear picture of your blood sugar levels is crucial.
What Is Diabetes And Prediabetes?
Type 2 diabetes is an impairment in the way the body regulates and uses sugar (glucose) as a fuel. For the development of the disease, there are primarily two interrelated problems at work. Your pancreas does not produce enough insulin — a hormone that regulates the movement of sugar into your cells — and cells respond poorly to insulin and take in less sugar. These insulin management concerns can start to occur years or decades before a formal diagnosis of diabetes.
Prediabetes is a serious health condition where blood sugar levels are higher than normal, but not high enough yet to be diagnosed as type 2 diabetes. The CDC estimates that more than 1 in 3— American adults have prediabetes with more than 80% unaware of their condition.
How Is Diabetes And Prediabetes Diagnosis?
There are several ways to diagnose diabetes. Each way usually needs to be repeated on a second day to confirm the diagnosis.
Measuring A1C:
The A1C test measures your average blood glucose for the past two to three months. The advantages of being diagnosed this way are that you don't have to fast or drink anything.
Your A1C test result is given in percentages. The higher the percentage, the higher your blood sugar levels have been:
A normal A1C level is below 5.7%
Prediabetes is diagnosed if the level is between 5.7 to 6.4%. Having prediabetes is a risk factor for getting type 2 diabetes.
Type 2 diabetes is diagnoses if a level is above 6.5%
Fasting Plasma Glucose (FPG):
This test checks your fasting blood glucose levels. Fasting means not having anything to eat or drink (except water) for at least 8 hours before the test. This test is usually done first thing in the morning, before breakfast.
A fasting glucose is only designed to measure glucose levels during the fasting period. It does not give a full picture of how a person’s body is handling sugar over a period of days or weeks. It does not provide any predictive insight into trends toward diabetes, prediabetes or other blood sugar handling issues. Fasting glucose levels can be highly affected by factors completely outside of diet such as poor sleep the night before or high stress levels.
Normal Fasting Glucose: less than 100 mg/dl
Prediabetes: 100 mg/dl to 125 mg/dl
Diabetes: 126 mg/dl or higher
Oral Glucose Tolerance Test (OGTT):
The OGTT is a two-hour test that checks your blood glucose levels before and two hours after you drink a special sweet drink. It tells the doctor how your body processes sugar.
Normal OGTT: Two-hour blood glucose less than 140 mg/dl blood
Prediabetes: Two-hour blood glucose of 140 to 199 mg/dl
Diabetes: Two-hour blood glucose of greater than or equal to 200 mg/dl
Random Plasma Glucose Test:
This test is a blood check at any time of the day when you have diabetes symptoms. Diabetes is diagnosed at a blood glucose of greater than or equal to 200 mg/dl.
What Are Optimal Glucose Levels?
In functional medicine, we are always looking beyond “normal” when it comes to lab marker ranges. When interpreting labs, “normal” does not necessarily equate to optimal if you are interested in preventing disease.
Optimal/Functional A1c Ranges:
Optimal Range for A1c: less than 5.3%
Less than Optimal/Pre-diabetic stage: A1c 5.4-6.0% (Your lab will call this “normal” but, in functional medicine we consider this a concerning zone.)
Sub-optimal: Any A1c above 6.0% reveals a problem with blood sugar control.
In functional medicine, and at Relish Health, we want to catch blood sugar issues as early on as possible. The A1c test offers us a window into your last 8-10 weeks of blood sugar balance. It gives us clues into how sugars may be affecting your cells and tissues and can predict if you may progress to having diabetes. Prediction is key to prevention when it comes to disease.
Health Effects of Chronically High A1c
The consequences of sub-optimal blood sugar balance over time include an increased risk of:
Cardiovascular disease including elevated blood pressure, increased risk of heart attacks and strokes, and even impotence
Diabetes
Increased annual brain shrinkage and risk for cognitive decline
What Causes A High A1c?
It is tempting to place all the blame for a high A1c levels on too much sugar in the diet. In reality, there are many lifestyle factors that can directly affect your A1c levels such as:
Sleep issues. Sleep deprivation is a leading causal factor behind blood sugar imbalances.
Stress. Chronic stress can trigger excessive stress hormones that raise blood sugar and can create insulin resistance.
Too many carbs, or too many of the “wrong” carbs. Excessive consumption of sugar and refined carbohydrates can trigger blood sugar imbalances. However, not all carbs will hurt you. “Good carbs” like those found in moderate amounts of whole fruits, vegetables and even sweet potatoes or white potatoes with the skins-on can be included in a healthy diet.
Artificial sweeteners. Artificial sweeteners like aspartame, sucralose and saccharin have recently been shown to affect blood sugar and insulin levels.
Not enough muscle mass and lack of exercise. Muscle helps your body regulate blood sugar. If you have a low lean muscle mass due to lack of exercise this could contribute to higher A1c levels.
Ways to Lower your A1c Levels
Relish Health can help you develop a personalized plan, but in general you can lower your A1c levels by:
Reducing your intake of refined carbs and sugar. Minimize consumption of pastries, bagels, breads, pastas, cereals, and candy. Focus on eating non-starchy vegetables, proteins, fats, and small amounts of whole grains, fruits, and starchy veggies like sweet potatoes or beets.
Increase your protein intake. Protein helps stabilize blood sugar while increasing satiety. Aim to have a small amount of lean animal or plant-based protein at every meal and snack. Relish Health can help you determine your protein needs with body composition analysis.
Exercise regularly. Focus on exercises that build muscle mass. High intensity interval training (HIIT), weight training, yoga, and other weight-bearing exercises are excellent choices.
Manage stress. This is one of the most profound things you can do to impact your blood sugar levels. Stress managing activities include exercising, listening to music, journaling, spending time with friends, laughing, meditation, spending time in nature and limiting your screen time.
Optimize your sleep. Aim for 7.5-9 hours of sleep a night. Sleeping less may cause your blood sugar balance to suffer.
How Often Should You Check Your A1c?
Physicians typically recommend patients with type 2 diabetes check their A1c every three to six months to ensure adequate treatment. At Relish Health, we believe in the same vigilance to make sure that your lifestyle changes are giving you the results you want. If your A1c level falls in the concerning zone, we will recommend you check your A1c progress at least every 6 months.
If your A1c level is currently at an optimal level, we recommend checking your A1c once a year or every other year as part of routine preventative care. Many lifestyle choices over time can influence insulin resistance and blood sugar imbalances. Knowing your A1c level empowers you to manage your blood sugar balance proactively before it ever has the chance to become disease.
House Smoked Salmon with Tarragon Aioli, pickled red onion and sweet lemon Rind
This recipe is inspired by an appetizer from a favorite restaurant. I had the dish three times!!! while on holiday because I was so obsessed with the delicious flavors. I’ve managed to recreate this favorite dish to share with you.
The recipe is easy, but it does require multiple steps. I assure you; this dip is worth the effort. Eating healthy doesn't mean sacrificing flavor or fun. This gluten and dairy free, low carb friendly recipe makes an elegant and nourishing appetizer to offer your guests. Best of all, this smoked salmon recipe does not require any special equipment.
This recipe is inspired by an appetizer from a favorite restaurant. I had the dish three times!!! while on holiday because I was so obsessed with the delicious flavors. I’ve managed to recreate this favorite dish to share with you.
The recipe is easy, but it does require multiple steps. I assure you; this dip is worth the effort. Eating healthy doesn't mean sacrificing flavor or fun. This gluten and dairy free, low carb friendly recipe makes an elegant and nourishing appetizer to offer your guests. Best of all, this smoked salmon recipe does not require any special equipment.
Smoked salmon dip with tarragon aioli, pickled red onion and sweet lemon rind from The Library in St. Petersburg, FL.
Smoked Salmon with Tarragon Aioli, Pickled Red Onion, and Sweet Lemon rind
Author: Erica Leazenby, MD
Time: 4 hours inactive time; 15-20 minutes cook time
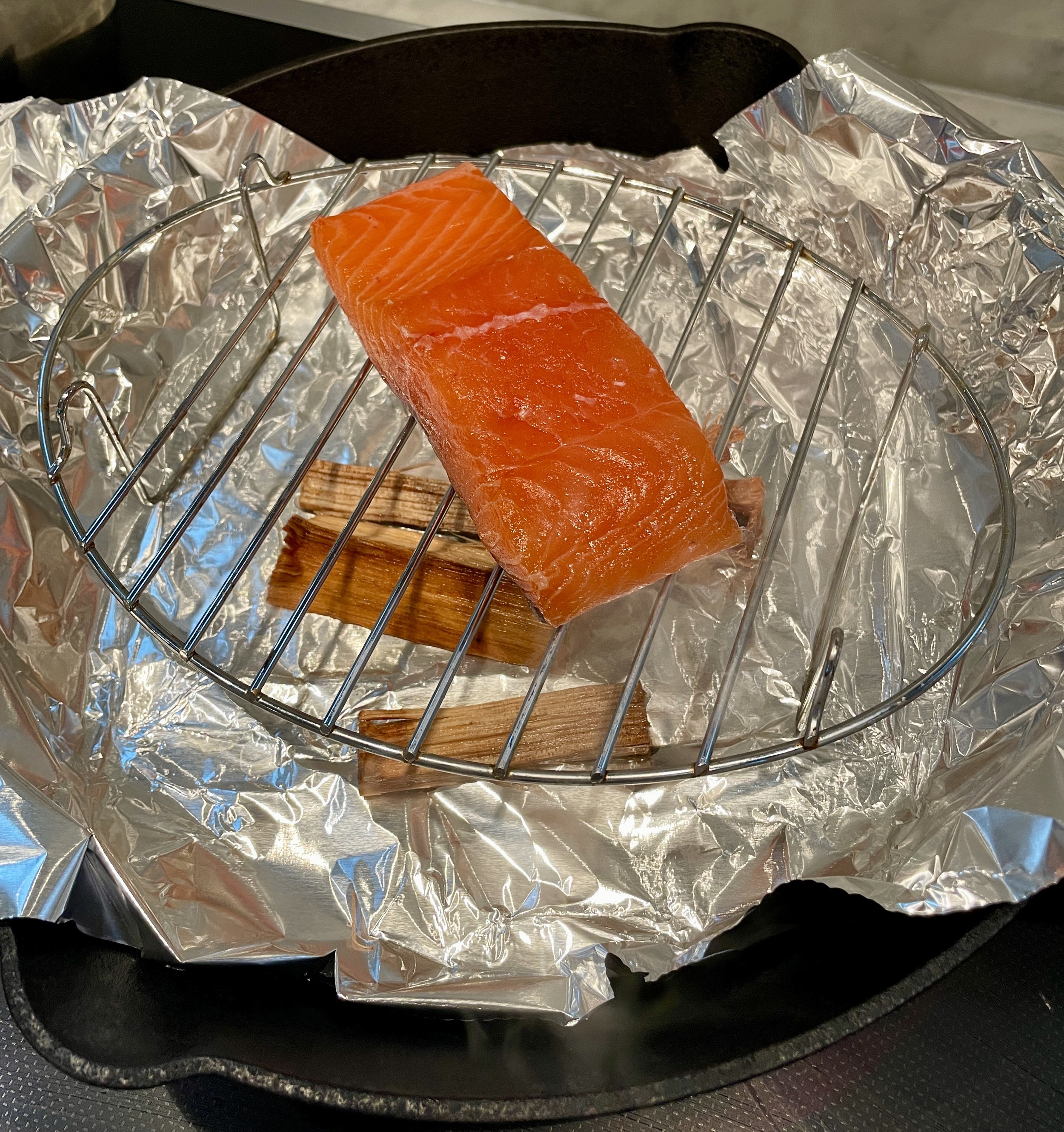
STEP 1: Brine and Smoke the Salmon:
Stovetop House smoked Salmon
Equipment:
Small, rimmed dish
Deep skillet such as a cast iron skillet, Dutch oven, or wok
Small grate that fits inside the skillet (like the grate often included with crock pots)
Aluminum foil
Ingredients:
8 Ounces wild caught Salmon
2 Tbsp sugar
2 Tbsp salt
Food grade wood chips
Directions:
Prepare the salmon: Mix the sugar and salt together. Place the salmon in a small, rimed dish. Spread the sugar and salt mixture over the salmon. Allow the salmon to brine for 1-4 hours, up to overnight. The longer you brine the salmon, the salty and firmer the fish may be. Rinse the brine off the salmon just prior smoking.
Place the food-grade, smoking wood chips in a bowl of water to soak at least 30 minutes prior to using. Consult the package of your wood chips for quantity needed. 1.5 to 2 tablespoons of superfine wood chips is often ideal, but your quality may vary depending on the size of your chips. If a quantity range is given on the package, I recommend using the lower quantity as you do not want the smoke to overwhelm the fish’s delicate flavor.
Line a deep skillet or wok with aluminum foil. Place the soaked wood on the foil. Heat the wood on medium-high heat until the wood starts to smoke.
Place the small wire grate over the wood in the skillet. Place the salmon on the grate. Use the aluminum foil to tent and seal the skillet. Once the skillet is sealed with foil, reduce the heat to medium-low.
Smoke the salmon for 10-20 minutes. Time will vary depending on the thickness of the fillet. Check the salmon at 10 minutes. Reseal the foil if the salmon needs additional smoke time. The salmon is done when the fish flakes easily or an instant-read thermometer reads 125 degrees.
The salmon can be served warm or at room temperature or can be used to make the dip list below.
STEP Two: Make the dip binder
Tarragon Aioli
This recipe makes more aioli than what is required for the salmon dip. The dip is delicious on roasted potatoes, as a veggie dip or smear on a sandwich. You will be grateful for the extra quantity.
Ingredients:
2 cloves garlic, minced
Pinch salt (about 1/8 tsp)
1 tablespoon minced fresh tarragon (about 2-3 large sprigs)
2 teaspoons lemon juice
1/2 cup avocado oil-based mayonnaise
Directions:
Mix all ingredients together. Store in an airtight container
Step Three: Prepare the garnishes:
Pickled Red Onion
Ingredients:
1 cup diced red onion
1/4 cup water
1/4 cup apple cider vinegar
1/2 tsp salt
1 Tablespoon sugar
1 bay leaf (optional)
1-2 allspice berries or a pinch of ground allspice (optional)
Directions:
Place the red onion is a heat safe bowl. Pour hot water over the onions. Let the onions sit in the water for a few minutes to remove bitterness and pungency.
Drain the red onions and place them in a glass jar. Add the water, vinegar, salt and sugar.
Store in the refrigerator up to several weeks.
Sweet Lemon Rind
Ingredients:
1 organic lemon
1 tablespoon sugar
1/4 teaspoon salt
Directions:
Slice the lemon thin. A mandolin held over a bowl works very well.
Place the shaved lemon in a jar with its juice. Add the sugar and sal.
Store in the refrigerator up to several weeks
Chopped Capers
Ingredients:
1-2 Tsp capers, rinsed and coarsely chopped
Directions: Garnish the dip with the capers.
Step Four: Put it all together:
Smoked Salmon with Tarragon Aioli
Ingredients:
8 ounces smoked salmon, skin removed
2 Tablespoons tarragon aioli
2 Tablespoons minced shallot
Directions:
Mix all ingredients in a mixing bowl. Chill the dip.
To serve, place the dip in a small serving bowl. Garnish the top of the dip with capers. Serve sweet lemon rind and pickles red onion on the side. Server the dip with crackers or sea salt flavored chips.
Other Salmon recipes:
HOUSE-CURED SALMON
SMOKED SALMON DIP
Relish Health Gift Guide 2023
It’s that time of year again when we think about how to show our love to family, friends and community. Gifts don’t necessarily come wrapped in a little box to make a big difference. Consider some of these options:
It’s that time of year again when we think about how to show our love to family, friends and community. Gifts don’t necessarily come wrapped in a little box to make a big difference. Consider some of these options:
The Gift of Time
Some of the most meaningful gifts are gifts of time.
We can volunteer. Being deliberate about calling or visiting our elders, cooking for people with stressful circumstances, pitching in to clean a park, serving meals at a shelter are just a few examples. Volunteering is good for your community and good for your soul and health.
We can spend time with someone we love. Time with friends and family is precious. It is not only enjoyable, but also contributes to better health. Finding time to enjoy the simple pleasures of the season with loved ones can help us feel more connected. My family loves to wander the local Christmas market, drive the neighborhood to view holiday lights and spend afternoons baking together.
We can make something for someone we love. Imagine how much your dear friend would love 2 quarts of soup or a soup assortment! Or a box of dark chocolate bark, a bag of homemade granola, delicious spiced biscotti or salted date caramel turtles all dolled up in a box with ribbon. A work of art, a lovingly knit cowl, or a hand-sewn sachet filled with lavender and rose petals fall into this category, too.
The Gift of Health
The New Year is a perfect time to renew focus on health. Consider giving devices or experiences that can gently help your loved ones reclaim healthy habits.
Wearable fitness devices are revolutionizing the way we monitor our health. I continue to marvel at the technology that is available for home use. If you or your loved one are driven by data, these devices can help you monitor and optimize your health trends. These are some of my top picks:
Created by neuroscientists and physicians, the Apollo wearable device delivers gentle, soothing vibrations, called Apollo Vibes™, that are like music your body can feel – higher vibrations improve your energy and focus, while lower vibrations reduce stress, help you relax and fall asleep.
The Oura Ring can be worn both day and night to capture activity, movement and sleep data. This data is used to calculate scores for “Readiness, Sleep, and Activity” giving you an accurate read on your overall health. The Oura Ring only uses Bluetooth during data downloads and can be safely used on a regular basis for those that are concerned about EMF exposure.
The Apple Watch has the capacity to monitor blood oxygen levels, electrocardiogram (ECG) and can provide notification for high and low heart rates or irregular heart rhythms. I personally use an Apple watch to monitor my steps, sleep pattern and daily heart rate variability (HVR).
Comprehensive lab and lifestyle assessment At Relish Health I have many tools to provide detailed evaluations of one’s nutritional status, hormone balance and stress levels to help make a personalized plan for optimal wellness. Learn more about available tests here.
The Gift of Wisdom
As a bookophile I believe books are always a great gift. These are a few books on my recently enjoyed list and wish list.
Creative Acts for Curious People “A delightful, compelling book that offers a dazzling array of practical, thoughtful exercises designed to spark creativity, help solve problems, foster connection, and make our lives better.”—Gretchen Rubin, New York Times bestselling author and host of the Happier podcast
The Art of Fermentation "The bible for the D.I.Y set: detailed instructions for how to make your own sauerkraut, beer, yogurt and pretty much everything involving microorganisms."--The New York Times
The Body Keeps the Score “Essential reading for anyone interested in understanding and treating traumatic stress and the scope of its impact on society.” —Alexander McFarlane, Director of the Centre for Traumatic Stress Studies
A GIFT For you… a jump start on a new you in the new year:
ProLon is a fasting mimicking diet system that gives you all the benefits of a 5-day fast while enjoying food. Increased focus, fat focused weight loss, enhanced cellular renewal and improved metabolic health are well documented benefits. (Learn more about the fast here.) Prolon kits can be purchased through Fullscripts or pick up at the Relish Health office.
Some gifts never go out of style. Check out the gift guides from
2018, 2019, 2020, 2021, and 2022
(This blog post is not sponsored by any manufacturer. However, at no cost to you, Relish Health may receive a commission on purchases made through an Amazon link.)
Lifestyle Supports for Seasonal Affective Disorder
Winter is here and many of us are confronting the long gray days that may take a toll on our mood. If you struggle with a low mood every winter, these strategies may make this winter a bit brighter.
Winter is here and many of us are confronting the long gray days that may take a toll on our mood. If you struggle with a low mood every winter, these strategies may make this winter a bit brighter.
What is Seasonal Affective Disorder (SAD)?
Seasonal affective disorder (SAD) is a mood disorder with depressive symptoms that occurs at specific times of year and fully resolves at other times of year. Most SAD occurs in the fall and winter. The cause of SAD is not fully understood, but theories implicate a shift in the circadian rhythm and alterations in serotonin in the brain as potential triggers. If you struggle with SAD, know that you are not alone. SAD affects 0.5% to 2.4% of the population at some point during their lifetime. Additionally, ten to 20% of people struggling with major depression will have a seasonal pattern consistent with SAD.
What are the risk factors for SAD?
Evidence for risk factors is limited, but some data suggests that family history, being female, younger adulthood, and living at a more northern latitude may increase your risk.
What are the symptoms of SAD?
SAD is a subtype of major depressive disorder. Symptoms include fatigue, loss of interest or pleasure in activities, mood swings, sadness, hopelessness, and social withdrawal among others. Recent studies suggest that SAD may have additional symptoms, including excessive sleepiness, increased appetite especially carbohydrate craving, and weight gain.
How can SAD be treated?
I recommend starting with a proper diagnosis. Before starting treatment, I recommend talking with Relish Health or your trusted healthcare provider about your symptoms. Ruling out underlying physical conditions such as anemia, vitamin deficiencies, hormone imbalances or other medical conditions is important for addressing the root cause of your mood.
Natural ways to improve SAD include:
Light Therapy, also called phototherapy, is a well-documented way to improve SAD. The therapy involves sitting a few feet from a special “light box” that exposures you to bright light within the first hour of waking each day. The recommended intensity of light is 2,500-10,000 lux. The time in front of the lamp will depend on the manufacture’s specification and your response to the light. Light boxes are about 20 times brighter than ordinary indoor light. They filter out the potentially damaging UV light, making them a safe treatment for most people. However, people with certain eye diseases or people taking certain medications that increase sensitivity to sunlight may need to use alternative treatments or use light therapy under medical supervision. Light therapy mimics natural outdoor light and appears to cause a change in brain chemicals linked to mood. Light therapy is one of the first line treatments for fall-onset SAD. It generally starts working in a few days to a few weeks.
Psychotherapy, also called talk therapy or cognitive behavior therapy, is another option to treat SAD. A trained metal health professional can help you identify and change negative thoughts and behaviors that may be making you feel worse. Optimizing stress management and learning healthy ways to cope with SAD can do wonders for your mood and long-term mental health.
Optimize vitamin D. Because many people with SAD often have vitamin D deficiency, nutritional supplements of vitamin D may help improve their symptoms. However, studies testing whether vitamin D is effective in SAD treatment have produced mixed findings, with some results indicating that it is as effective as light therapy but others detecting no effect.
Eat an anti-inflammatory diet. A nourished brain is a resilient brain. We need to consume several vitamins, minerals, fats, and antioxidants to feel our best, and the only way to authentically do that is with real food. Eat a balance of vegetables, well-sourced fish and poultry, starchy tubers (potatoes, sweet potatoes), fermented foods (sauerkraut, yogurt), nuts, seeds, fruits, and plenty of healthy fats such as olive oil, avocado, coconut oil, and fatty fish like salmon or sardines. If you think you are suffering from SAD, then avoid sugar, refined carbs (i.e., bread, crackers, pasta, cookies), and inflammatory oils, such as canola oil and see if this makes any difference in your mood. Research in the field of nutritional psychiatry shows that eating fish at least once or twice a week can decrease your risk of depression and avoiding ultra processed foods(UPFs) (ie. packaged snacks and frozen meals) and artificial sweeteners is important. People eating nine or more servings per day of UPFs had a 50% higher risk of developing depression than those consuming four or fewer servings per day (that bag of chips is likely multiple servings).
Keep moving. Commit to doing something quick, free, easy, convenient, and pleasant for a least a few minutes most days of the week. Exercise is like medicine. Even small amounts can deliver antidepressant benefits. I assure you doing something—no matter how small—is so much better than nothing. A new study published in 2023 found that weekly hot yoga reduced depressive symptoms by at least 50 percent. Approximately 44 percent of depressed participants of the study doing yoga weekly after 8 weeks were considered to be in remission from their depression.
Medicate or supplement wisely. Because SAD, like other types of depression, is associated with disturbances in serotonin activity, antidepressant medications or targeted supplements have their place in treatment regimens. I always recommend starting with good nourishment and self-care but talk to your healthcare provider or Relish Health if additional support is needed.
Learn more:
LIFESTYLE TIPS TO EASE YOUR ANXIETY
USE YOUR FORK TO IMPROVE YOUR FEELINGS
GOOD MOOD FOOD
References:
Galima SV, Vogel SR, Kowalski AW. Seasonal Affective Disorder: Common Questions and Answers. Am Fam Physician. 2020 Dec 1;102(11):668-672. PMID: 33252911.
Campbell PD, Miller AM, Woesner ME. Bright Light Therapy: Seasonal Affective Disorder and Beyond. Einstein J Biol Med. 2017;32:E13-E25.
MayoClinic.org. Seasonal affective disorder (SAD), Last accessed 11/25/2023.
The National Institute of Mental Health. Seasonal Affective Disorder. NIH Publication No. 20-MH-8138. Last accesses 11/25/2023.
Yang Y, Kim Y, Je Y. Fish consumption and risk of depression: Epidemiological evidence from prospective studies. Asia Pac Psychiatry. 2018 Dec;10(4):e12335. doi: 10.1111/appy.12335. Epub 2018 Sep 20. PMID: 30238628.
Li F, Liu X, Zhang D
Fish consumption and risk of depression: a meta-analysis
J Epidemiol Community Health 2016;70:299-304.
Samuthpongtorn C, Nguyen LH, Okereke OI, et al. Consumption of Ultraprocessed Food and Risk of Depression. JAMA Netw Open. 2023;6(9):e2334770. doi:10.1001/jamanetworkopen.2023.34770
Nyer MB, Hopkins LB, Nagaswami M, Norton R, Streeter CC, Hoeppner BB, Sorensen CEC, Uebelacker L, Koontz J, Foster S, Dording C, Giollabhui NM, Yeung A, Fisher LB, Cusin C, Jain FA, Pedrelli P, Ding GA, Mason AE, Cassano P, Mehta DH, Sauder C, Raison CL, Miller KK, Fava M, Mischoulon D. A Randomized Controlled Trial of Community-Delivered Heated Hatha Yoga for Moderate-to-Severe Depression. J Clin Psychiatry. 2023 Oct 23;84(6):22m14621. doi: 10.4088/JCP.22m14621. PMID: 37883245.
(This blog post is not sponsored by any manufacturer. However, at no expense to you, Relish Health may receive a commission on purchases made through an Amazon link.)
S'more Cupcakes
This week is a birthday week at my house. I strongly believe that life is meant to be celebrated, but not at the expense of feeling unwell. In our household, three out of four of us eat gluten and dairy free to ensure we feel our best. Over the years, I've become adept at creating gluten-free, dairy-free, and (mostly) refined sugar-free treats that are both indulgent and perfect for celebrations. These cupcakes have a delightful graham cracker-like flavor, thanks to the cinnamon and honey, which pairs beautifully with the rich chocolate frosting and toasted marshmallow. The recipe is too good not to share!
This week is a birthday week at my house. I strongly believe that life is meant to be celebrated, but not at the expense of feeling unwell. In our household, three out of four of us eat gluten and dairy free to ensure we feel our best. Over the years, I've become adept at creating gluten-free, dairy-free, and (mostly) refined sugar-free treats that are both indulgent and perfect for celebrations. These cupcakes have a delightful graham cracker-like flavor, thanks to the cinnamon and honey, which pairs beautifully with the rich chocolate frosting and toasted marshmallow. The recipe is too good not to share!
S’more Cupcakes with Chocolate Fudge Frosting and Toasted Marshmallow
Author: Erica Leazenby, MD (cake adapted from Sweet Laurel)
Makes: 10 cupcakes
Ingredients:
Frosting:
4 ounces semi-sweet or dark chocolate chips (allergen friendly if needed)
1/4 cup coconut oil
1/2 cup smooth unsweetened almond butter
Garnish:
10 large marshmallows
Cake:
2 1/2 cups almond flour
1/2 tsp baking soda
1/2 tsp sea salt
2 1/2 tsp ground cinnamon
2 eggs
1/4 cup coconut oil, melted
1/2 cup honey
1 tsp vanilla extract
Directions:
For the graham cracker flavored cupcakes:
Preheat the oven to 350 degrees F (or 325 degrees F if using the convection setting).
Line your muffin tins with cupcake liners.
Combine the almond flour, baking soda, salt, and cinnamon; mix well. In a separate bowel, combine the eggs, coconut oil, honey and vanilla. Whisk the wet ingredients until they are well incorporated. Add the wet ingredient to the dry ingredients and mix until a batter is formed. Divide the batter evenly among the 10 cupcake liners.
Bake the cupcakes for approximately 20-25 minutes or until a toothpick inserted into the middle of the cupcake comes out clean. Allow the cupcakes to cool to room tempature.
For the frosting:
Place the chocolate chips and coconut oil in a microwave safe bowl. Heat the mixture in the microwave in 15-30 second increments, stiring frequently, until the chips are nearly completely melted. Remove the mixture from the microwave. Continue to stir the chocolate until it is smooth and all the chips have completely melted. Take care to not overheat the chocolate.
Once the chocolate mixture is complete smooth, add the almond butter. Stir until well combined.
Allow the frosting to cool.
For soft, spreadable frosting, allow the frosting to cool to room temperature.
For more firm frosting that can be piped, cool the frosting in the refrigerator until it is firm, but not hard. This may take 15-45 minutes depending on the starting temperature.
Garnish:
Preheat the over broiler.
Place the 10 marshmallows on a parchment paper lined baking sheet.
Place the baking sheet on the top shelf of the oven. Toast the marshmallows to desired color, about 20-30 seconds. Watch closely.
Allow to cool.
Putting it all together:
Top the cupcakes with chocolate frosting once they are completely cool. Garnish with a toasted marshmallow. Enjoy.
More gluten and dairy free treats:
A PRIMER ON GLUTEN-FREE FLOURS
GLUTEN & DAIRY FREE GINGERBREAD BISCOTTI
BANANA PECAN BREAKFAST BREAD
GRAIN-FREE CHOCOLATE ZUCCHINI MUFFINS
Nourishing Your Bones: Essential Steps for Optimal Bone Health
Bones form the scaffold of our bodies, providing structural support, protecting vital organs, and serving as reservoirs for essential minerals. Beyond their mechanical role, bones are living tissues, constantly undergoing remodeling and regeneration. It is easy to take our skeleton for granted, but understanding the pivotal importance of bone health has profound implications for longevity, mobility, and the overall vitality of the human body.
How to provide optimal care for your bones:
Bones form the scaffold of our bodies, providing structural support, protecting vital organs, and serving as reservoirs for essential minerals. Beyond their mechanical role, bones are living tissues, constantly undergoing remodeling and regeneration. It is easy to take our skeleton for granted, but understanding the pivotal importance of bone health has profound implications for longevity, mobility, and the overall vitality of the human body.
How to provide optimal care for your bones:
Avoid Processed and Ultra Processed Foods: One of the most impactful steps you can take to support your bone health is to steer clear of processed and ultra processed foods. Ultra-processed foods are made mostly from substances extracted from foods, such as fats, starches, and added sugars. They may also contain additives like artificial colors and flavors or stabilizers while lacking the essential nutrients needed for bone strength. Examples of these foods are frozen meals, soft drinks, hot dogs and cold cuts, fast food, packaged cookies, cakes, and salty snacks. Opt for whole, minimally processed foods like fresh fruits, vegetables, lean proteins, and whole grains.
Eat Your Vegetables: Beyond their culinary appeal, vegetables are rich in a variety of vitamins and trace minerals crucial for bone health. Incorporate a colorful array of vegetables into your dishes to ensure you're getting a wide range of nutrients like vitamin C, potassium, and antioxidants, which all play a role in maintaining healthy bones.
Eat Adequate Calcium, Vitamin D and Supporting Nutrients: Calcium and vitamin D are cornerstones of bone health, and without them, our bones can become weak and brittle. For the dairy tolerant, yogurt, small amounts of cheese and judicious consumption of milk can be good sources of calcium. Dairy-free sources of calcium include leafy greens like kale and collard greens, almonds, and fortified non-dairy milks. Ensure you're getting enough sunlight exposure for natural vitamin D synthesis, and incorporate vitamin D-rich foods like fatty fish and fortified products. Many people also benefit from additional vitamin D supplementation. Checking vitamin D blood levels periodically can help you determining if supplementation is right for you. Additionally, it's crucial to include supporting nutrients like magnesium and vitamin K2 in the diet, which aid in calcium absorption and bone mineralization. Foods rich in vitamin K and magnesium include leafy greens, broccoli, nuts, seeds, and fermented soy products.
Eat Adequate Protein: Protein is essential for bone health, as it provides the building blocks necessary for bone tissue repair and growth. Include a variety of lean proteins such as poultry, fish, and plant-based protein options like legumes, quinoa and tofu to support optimal bone health. Aim for 1.0 to 1.3 g/kg body weight per day. (For example a 150 pound or 68 kg female should aim for 68-88 grams of protein per day.)
Optimize Gut Health: A healthy gut is crucial for absorbing the nutrients needed for bone health. Addressing issues like reflux, irregular bowel movements and bloating can significantly improve nutrient absorption. Consider incorporating gut-friendly foods like fermented vegetables, kefir, and bone broth into your meals. Additionally, focus on identifying and eliminating potential trigger foods that may be contributing to digestive discomfort.
Manage Stress: Stress can have a significant impact on bone health, as chronic stress can lead to increased levels of cortisol, which can weaken bones over time. Stress management techniques such as mindfulness, deep breathing exercises, and regular physical activity are important additions to your daily routine. These practices not only support mental well-being but also contribute to the overall health and resilience of your bones.
Get Adequate Exercise: Regular weight-bearing and resistance exercises are crucial for maintaining bone density and strength. Activities like walking, jogging, weight lifting, and yoga are excellent choices. Aim for a minimum of 150 minutes of movement per week.
Relish Health is here to help you support your bones through nutritional counseling and targeted testing of nutrients, gut health, hormones and metabolism.
Understanding the Gut-Skin Connection: Fixing your Skin From The Inside Out
The skin is the largest and most external barrier of the body with the outer environment. It is richly perfused with immune cells and heavily colonized by bacteria. These microbes help train the body’s immune cells and help determine overall well-being. The skin has a unique microbiome that is distinct from the gut microbiome, yet scientists are learning that there is a strong bidirectional relationship between the health of these two areas of the body. The relationship is often termed the “gut-skin axis.”
Integrative dermatology is a relatively new field that combines conventional dermatology with functional medicine principals to diagnose and treat skin conditions. It takes a holistic approach to skincare and skin conditions, recognizing that the skin's health is influenced by various factors, including nutrition, stress levels, and overall well-being. Integrative dermatology focuses on treating the whole person, rather than just the skin condition, and aims to provide comprehensive and effective treatment options for patients by addressing the underlying causes of skin issues considering the physical, biological, psychological, social, and environmental factors that affect the lives of patients with dermatological diseases.
The human body is home to ecosystems of bacteria, yeast, viruses and other organisms that inhabit different regions of our body. These ecosystems are often collectively called the microbiome. While specific species and strains of organisms vary based on location in the body, imbalances of organisms in any given site play a role in the health of the body as a whole. The microbiome is a key regulator for the immune system. Hence, imbalances (also called dysbiosis) of these organisms are associated with an altered immune response, promoting inflammation in potentially multiple areas of the body. (1) A dysbiosis can occur if there are too many “bad” species, not enough “good” species, or not enough diversity of species.
The skin is the largest and most external barrier of the body with the outer environment. It is richly perfused with immune cells and heavily colonized by microbial cells. These microbes help train the body’s immune cells and help determine overall well-being. The skin has a unique microbiome that is distinct from the gut microbiome, yet scientists are learning that there is a strong bidirectional relationship between the health of these two areas of the body. The relationship is often termed the “gut-skin axis.” Skin conditions including rosacea, acne, psoriasis, atopic dermatitis, skin aging and others are often associated with altered gut microbiome health.
The gut and skin connection
The intestinal tract houses a diverse collection of bacteria, fungi, and protozoa. Many of these microorganisms are essential for metabolic and immune function. An imbalance in this microbiome can result in a breakdown of gut barrier function resulting in antigenic food proteins and bacteria components entering the body’s circulation to trigger inflammation. This inflammation can affect many organs, including the skin.
Adult Acne Vulgaris
Acne is a skin condition that occurs when your hair follicles become plugged with oil and dead skin cells. Acne can be described as whiteheads, blackheads, pimples or deep cysts. Cystic acne is linked to the health of the skin’s microbiome, in particular the balance of a bacteria called Cutibacterium acnes. In a diverse, balanced skin microbiome, this bacterium is involved in maintaining a healthy complexion. However, if there is loss of the skin microbial diversity, this bacteria can also trigger cystic acne. The microbial imbalance can lead to the activation of the immune system and a chronic inflammatory condition like acne. (2) Like in the gut, the health of the skin microbiome influences the release of chemicals triggering inflammation. Optimizing both the gut microbiome and skin microbiome are important stratagies to resolve acne by controlling inflammation both at the skin level and whole body level.
Rosacea
Rosacea is a common, chronic inflammatory skin condition that causes flushing, visible blood vessels and small, pus-filled bumps on the face. The exact cause of rosacea is debated and likely related to multiple factors. Like acne, the skin microbiome and its associated inflammatory effects plays a role in rosacea's etiology. There are also numerous studies connecting rosacea to gastrointestinal disorders including celiac disease, inflammatory bowel disease, irritable bowel syndrome, Helicobacter pylori infection and small bowel bacterial overgrowth.(3) Conventional treatment of rosacea often involves managing symptoms. Identifying and addressing potential associated gut-related illnesses is an effective tool to help support rosacea management.
Eczema
Eczema, also called atopic dermatitis, is a chronic condition that makes skin red and itchy. It is common in children but can occur at any age. Atopic dermatitis tends to flare periodically and is often associated with asthma or allergies. Atopic dermatitis is the most common inflammatory skin disease affecting 7% of adults and 15% of children.(1)
Studies have shown that atopic dermatitis is associated with lower gut microbiome diversity, lower levels of beneficial species, such as Bacteroidetes, Akkermansia, and Bifidobacterium in the gut, and higher amounts of harmful bacteria species including Staphylococcus aureus on the skin.(1) The intestinal microbiome modulates the body’s immune system and inflammatory responses and thus may play a role in the development of eczema and its treatment. Targeted probiotics can play a role in prevention and treatment of this disease.(4)
Psoriasis
Psoriasis is an inflammatory, autoimmune skin disease that causes a rash with itchy, scaly patches, most commonly on the knees, elbows, trunk and scalp. The illness is associated with an intimate interplay between genetic susceptibility, lifestyle, and environment. People with psoriasis have an increased risk to develop intestinal immune disorders, such as inflammatory bowel disease like ulcerative colitis and celiac disease.(1) A growing body of evidence highlights that intestinal dysbiosis is associated with the development of psoriasis.(5) One study showed that malabsorption of nutrients in the gut was more prevalent among patients with psoriasis. Celiac disease, bacterial overgrowth, parasitic infestations and eosinophilic gastroenteritis could be possible causes of malabsorption in these patients.(6) Addressing associated gut conditions may play a role in management of symptoms.
Skin Aging
Skin aging is associated with multiple degenerative processes including oxidation and inflammation. Multiple factors including diet, UV exposure, and environment play a role in the regulation of the aging process. New research shows that healthier diets are linked to fewer signs of skin aging.(7) Additionally, oral probiotics may play a role in regulating skin aging through influences on the gut-skin axis. In a study published in 2015, the oral probiotic Lactobacillus plantarum HY7714 was shown to improve skin hydration, skin elasticity and UV related skin changes.(8)
Skin Care may need to Start with Gut Care
Optimizing the gut microbiome has a role in addressing skin disorders. The following strategies can improve the microbiome:
Eat better. The microbiome is influence by the food we eat. Beneficial bacteria thrive on fiber that comes from eating a variety of vegetables regularly. The growth of unfavorable bacteria is influenced by sugar, saturated fats and a lack of fiber/vegetables in the diet. To optimize your microbiome, avoid refined sugar and saturated fats like those found in sodas, breakfast cereals, candies, cakes, red meat (limit to 1 or 2 servings a week to prevent overconsumption) and what is commonly referred to as “junk food”.
Use antibiotics wisely. Antibiotic treatment is necessary from time to time. However antibiotics can significantly lower microbiome diversity and the quantity of beneficial bacteria.(9) When prescribed an antibiotic, ask your health care provider if it is truly necessary. Speak with your provider about using prebiotics and probiotics to support the microbiome after the antibiotic use.
Repair the gut flora. In addition to a fiber-rich diet, probiotics may play a role in optimizing gut function. Probiotic science is in its infancy, but there is research suggesting that certain strains may benefit certain medical conditions. Speak with your health care provider for probiotic recommendations that may best suit your medical needs.
Identify other ways to care for your digestive system, such as repairing the wall of the small intestine which may have been irritated by a poor diet, poor digestion, medications or stress. Identifying food sensitivities, restoring nutritional deficiencies and eating adequate nutrients to support healing are important.
Many of the interventions above can be easily implemented without need for laboratory tests. There are no specific gastrointestinal lab markers that are known to directly cause skin issues. However, assessments of the GI system may reveal abnormalities indirectly impacting skin health. Relish Health relies on multiple tools such as stool microbiome testing, breath tests and food sensitivity tests to understand the health of the gut-skin axis and develop targeted interventions to address gut and skin conditions.
A PRIMER ON HISTAMINE INTOLERANCE
TESTING, TESTING... WHICH ONES MIGHT BE RIGHT FOR YOU?
References:
De Pessemier B, Grine L, Debaere M, Maes A, Paetzold B, Callewaert C. Gut–Skin Axis: Current Knowledge of the Interrelationship between Microbial Dysbiosis and Skin Conditions Microorganisms. 2021 Feb; 9(2): 353. doi: 10.3390/microorganisms9020353
Dréno B,. Pécastaings S, Corvec S, Veraldi S, Khammari S, Roques C. Cutibacterium acnes (Propionibacterium acnes) and acne vulgaris: a brief look at the latest updates. J Eur Acad Dermatol Venereol 2018 Jun;32 Suppl 2:5-14. doi: 10.1111/jdv.15043.
Daou H, Paradiso M, Hennessy K, Seminario-Vidal L. Rosacea and the Microbiome: A Systematic Review. Dermatol Ther. 2021 Feb;11(1):1-12. doi: 10.1007/s13555-020-00460-1.Epub 2020 Nov 10.
Fiocchi A, Pawankar R, Cuello-Garcia C, et. al. World Allergy Organization-McMaster University Guidelines for Allergic Disease Prevention (GLAD-P): Probiotics World Allergy Organ J. 2015; 8(1): 4. Published online 2015 Jan 27. doi: 10.1186/s40413-015-0055-2
Sikora M, Stec A, Chrabaszcz M, Knot A, Waskiel-Burnat A, Rakowska A, Olszewską M, Rudnicka L. Gut Microbiome in Psoriasis: An Updated Review. Pathogens. 2020 Jun; 9(6): 463. Published online 2020 Jun 12. doi: 10.3390/pathogens9060463
Ojetti V, De Simone C, Sanchez J, Capizzi R, Migneco A, Guerriero C, Cazzato A, Gasbarrini G, Pierluigi A, Gasbarrini A. Malabsorption in psoriatic patients: cause or consequence? Scand J Gastroenterol. 2006 Nov;41(11):1267-71.
doi: 10.1080/00365520600633529.
Katta R, Sanchez A, Tantry E. An Anti-Wrinkle Diet: Nutritional Strategies to Combat Oxidation, Inflammation and Glycation. Skin Therapy Lett. 2020 Mar;25(2):3-7.
Lee, D. E. et al. (2015) “Clinical Evidence of Effects of Lactobacillus plantarum HY7714 on Skin Aging: A Randomized, Double Blind, Placebo-Controlled Study,” Journal of Microbiology and Biotechnology. Journal of Microbiology and Biotechnology. https://doi.org/10.4014/jmb.1509.09021
Ramirez J. Guarner F, Fernandez, L, Maruy A, Sdepanian V, Cohen H. Antibiotics as Major Disruptors of Gut Microbiota. Front. Cell. Infect. Microbiol., 24 November 2020 | https://doi.org/10.3389/fcimb.2020.572912
Stubbe C. The Gut Microbiome in Dermatology. Anti-aging Medical News. Spring 2022. p76-80.
Grain-Free Chocolate Zucchini Muffins
The squash plants in my garden have yielded an incredible amount of fruit this year. I've been creative in utilizing this bounty: crafting sautéed zucchini with caramelized onions and oregano, preparing zucchini fritters, incorporating zucchini into turkey meatballs and burgers, concocting zucchini fried rice, sharing the surplus with my neighbors, and even relishing zucchini muffins! While I've managed to gather most zucchinis when they're small and tender, inevitably there are a few that escape notice and grow larger below the garden foliage. This recipe proves excellent for utilizing such oversized produce; just remember to remove any seeds.
The squash plants in my garden have yielded an incredible amount of fruit this year. I've been creative in utilizing this bounty: crafting dinner sides of sautéed zucchini with caramelized onions and oregano, preparing zucchini fritters, incorporating zucchini into turkey meatballs and burgers, concocting zucchini fried rice, sharing the surplus with my neighbors, and even baking zucchini muffins! While I've managed to gather most zucchinis when they're small and tender, inevitably there are a few that escape notice and grow larger below the garden foliage. This recipe is excellent for utilizing the oversized produce; just remember to remove any large seeds.
These muffins fall within the realm of indulgence due to the addition of maple syrup (yep, it's still added sugar), yet they maintain a notably lower sweetness level compared to numerous renditions of zucchini quick breads. The inclusion of almond butter also introduces some wholesome, polyunsaturated fats, imparting a hint of virtuousness to the muffins.
Grain-Free Chocolate Zucchini Muffins
Author: Erica Leazenby, MD (Inspired by Pamela Salzman)
Makes: 12 muffins
Time: 35 minutes
Ingredients:
Coconut oil for greasing the muffin pan
1 cup creamy, unsweetened, unsalted almond butter, raw or roasted
2 cups of shredded zucchini, about 1 medium zucchini (do not squeeze out excess liquid)
1/3 cup pure maple syrup
¼ cup cocoa powder
¼ teaspoon fine ground sea salt
1.5 teaspoon baking soda
2 large eggs
1 teaspoon pure vanilla extract
1/2 cup dark or semi-sweet chocolate chips
Directions:
Preheat your oven to 350 degrees (or 325 convection). Grease and/or line your muffins tins.
In a large bowl combine all the ingredients.
Divide the batter evenly into the prepared muffin pan and bake until just set and a toothpick comes out clean or with dry crumbs. Do not overbake. Standard size muffins will take about 20-25 minutes to bake.
Allow to cool before serving.
Estimated nutritional value per muffin: Total Calories 221, Total Fat 17.5g, Carbs 19g, Fiber 2g, Protein 5g
Other Gluten-free Treat Recipes:
PECAN BANANA BREAKFAST BREAD
TOASTED MARZIPAN
GLUTEN & DAIRY FREE GINGERBREAD BISCOTTI
The Hearty, Semi-homemade, Summer Chop Salad
I might be revealing my age here, but I have fond memories of tuning into the show "Semi-Homemade Cooking with Sandra Lee" during my younger years. Does anyone else here recall her ingenious transformations of ordinary grocery items into fancy meals? Drawing inspiration from that very concept, I've put together a salad that encapsulates those creative culinary endeavors.
If you're looking for a dish that's not only a treat for your taste buds but also a testament to the art of culinary resourcefulness, give this chopped salad a try.
I might be revealing my age here, but I have fond memories of tuning into the show "Semi-Homemade Cooking with Sandra Lee" during my younger years. Does anyone else here recall her ingenious transformations of ordinary grocery items into fancy meals? Drawing inspiration from that very concept, I've put together a salad that encapsulates those creative culinary endeavors.
My culinary canvas showcases a blend of both sweet and savory vegetables. I’ve mixed caramelized roasted sweet potatoes, aromatic herbed chickpeas, earthy sliced beets, umami-rich salty prosciutto, and vibrant roasted red peppers. However, let your imagination roam free— the combination of additional veggies and flavors is endless. Incorporating an array of diverse vegetables not only elevates the flavor profile of your salad but also increases the density of nutrients and fiber types, promoting optimal health.
So, if you're looking for a dish that's not only a treat for your taste buds but also a testament to the art of culinary resourcefulness, give this chopped salad a try.
The Hearty, Semi-homemade Summer Chop Salad
Author: Erica Leazenby, MD
Time: 20-30 minutes
Serves: 6-8 people
Dressing:
1/2 cup olive oil
1/4 cup balsamic vinegar
1 tsp Dijon mustard
Salt and pepper to taste
Ingredients:
Olive oil
Salt and pepper
1 large sweet potato, diced into 1 cm cubes
3 romaine hearts, washed and diced into bite size pieces
1 roasted red pepper from a jar, diced or cut into strips
1 cup chickpeas, plain or herbed (leave off is following a paleo or whole 30 diet)
1 cup beets, diced (freshly roasted or from a can or package)
6-8 prosciutto slices, cut into strips (Speck or uncured diced salami are also great options.)
Other optional add-ins: diced cooked uncured bacon, diced chicken, canned salmon, hard boiled egg, sunflower seeds, sliced olives, feta…
Directions:
Wash and dice the sweet potato. Drizzle lightly with olive oil and season with salt and pepper. Roast the sweet potato in a 400 degree pre-heated over or air fried for 12-15 minutes or until starting to brown.
While the sweet potato is roasting, wash, dry and dice the romaine.
Add the additional diced ingredients to the salad greens including, roasted red pepper, chickpeas, beets, and prosciutto.
Prepare the dressing.
Once the sweet potatoes have finished roasting and have cooled to room temperature they can be added to the salad.
Toss all the salad ingredients together. Dress the salad as a whole or dress individual portions*.
* Undressed salad will keep in the refrigerator for several days. This makes an excellent make-ahead lunch. Add the dressing just prior to eating.
How to Calculate Your Ideal Protein Needs
Protein is a macronutrient that is essential for the growth, repair, and maintenance of the body's tissues and organs. Protein needs depends on various factors such as your age, sex, weight, physical activity level, and overall health goals. Consider the following benefits of adequate protein:
Protein 101
Protein is a macronutrient that is essential for the growth, repair, and maintenance of the body's tissues and organs. It is made up of smaller units called amino acids, which are linked together in various sequences to form different types of proteins. There are 20 different amino acids, and the specific arrangement of these amino acids determines the structure and function of each protein. Of these amino acids, 9 are considered essential—meaning your body cannot synthesize them—so you must get them from food.
Protein is obtained through the diet from various sources, including animal products like meat, fish, eggs, and dairy, as well as plant-based sources such as beans, lentils, nuts, and seeds. It is an essential part of a balanced diet and is required for overall health and wellbeing.
How Much Protein Do You Need?
Protein needs depends on various factors such as your age, sex, weight, physical activity level, and overall health goals. According to the U.S. government, the recommended daily allowance (RDA) for protein intake is 0.8 grams of protein for each kilogram of body weight, or 0.36 grams per pound of body weight. For a 140 pound woman, for example, this translates to 50 grams of protein or the amount in a 6-ounce portion of chicken breast.
However, this is a basic guideline and may not be sufficient for everyone. Most experts agree that the RDA’s protein recommendation is woefully inadequate for optimal health. The RDA reflects the basic need of a sedentary individual to prevent illness. Individuals who are more physically active, athletes, pregnant or lactating women, and older adults may require higher protein intake. For example, athletes and those engaged in intense physical activity might need 1.2 to 2.2 grams of protein per kilogram (0.55-1 grams per pound) of body weight per day to support muscle repair and growth.
For older adults (generally defined as over 60 years old), increasing protein intake to 1.2 to 1.6 grams per kilogram (0.55-0.73 grams per pound) of body weight may be beneficial, as protein plays a crucial role in preserving muscle mass and overall health during aging.
Benefits of Eating Adequate Protein
Weight management during perimenopause: Prioritizing protein during perimenopause and menopause may ward off weight gain. The research suggests that the body's appetite for protein increases during perimenopause (due to hormonally-induced tissue protein breakdown) but if protein requirements are not met, women over-consume other forms of energy. A diet rich in protein, coupled with regular exercise, especially strength training, can help regenerate muscle mass. More muscle mass contributes to a faster metabolism, aiding in weight management during menopause.
Age better with more protein: Getting enough protein is emerging as a key factor in successful aging. As people age, protein becomes even more crucial as it helps maintain muscle mass, supports immune function, and aids in overall tissue repair and maintenance. Studies by experts indicate that after age 40, muscle mass may decrease by up to 8% every decade, potentially resulting in a 16% loss of muscle mass for postmenopausal women by age 60. Beyond age 60, the rate of muscle mass loss further accelerates to around 10 to 15% per decade. This decline in muscle mass often leads to sarcopenia, a condition characterized by weak muscles, frailty, and reduced mobility. Numerous clinical studies have demonstrated that consuming adequate protein can help counteract unwanted muscle loss and weakness, promoting better overall health and physical function. Research suggests that for older adults, protein intake of around 1.2 to 1.6 grams per kilogram (0.54 to 0.73 grams per pound) of body weight per day supports healthy aging and preserve muscle mass. For example, if an older adult weighs 70 kilograms (154 pounds), their protein intake may range from approximately 84 to 112 grams per day.
Reduce your risk of dementia: According to recent studies, adults over age 65 may have healthier brains if protein intake is at least double the RDA, or 1.6 grams per kilogram of body weight, or 0.73 grams per pound.
The precise way in which protein supports the aging brain remains uncertain. It could involve a direct mechanism, such as supplying specific amino acids essential for enhancing neurotransmitters. Alternatively, protein intake might indirectly benefit the brain by averting muscle loss and frailty, which could otherwise result in a less dynamic and engaged brain-healthy lifestyle. Regardless of the exact mechanism, individuals who retain muscle mass as they age generally exhibit more robust brain health.
The Cache County Dementia Progression Study showed a strong association between low protein intake and dementia. In fact, the lower the intake, the more severe the dementia.
In this older study of adults over 65, higher protein intake was positively associated with memory function. Those adults with the highest protein intake also had the lowest incidence of mild cognitive impairment.
In this study published in the Journal of Alzheimer’s Disease, healthy older adults with a high protein (and fiber) intake had less amyloid-β accumulation in the brain, when compared to those with medium to low intake. In fact, those in the lowest tier of protein intake were 12 times more likely to have a high burden of amyloid protein visualized on brain imaging studies.
Is It Harmful to Eat Too Much Protein?
The belief that excessive protein consumption leads to kidney problems or other health issues is a misconception. Long-term consumption of protein at 2 grams per kilogram body weight per day (or 0.9 grams per pound per day) is safe for healthy adults. Nevertheless, individuals with specific kidney conditions should consult their doctors about the most appropriate protein intake. Protein that isn't utilized for muscle development or other bodily functions is efficiently eliminated through the kidneys as urea.
In summary, it's wiser to lean towards consuming more protein than insufficient amounts. Achieving an optimal protein intake is essential for both your body and cognitive health as you grow older.
How To Complete An Elimination Diet Suited To You
Elimination diets are commonly used tools in functional medicine. The food we eat is the foundation of our wellness yet, some foods, even seemingly healthy ones, may triggers unwanted symptoms in some people. It is estimated that between 2–20% of people worldwide may suffer from some form of a food intolerance. An elimination diet is the process of removing a food or group of foods from a person’s diet for a set period of time. The absence of the food(s) and then careful reintroduction of the item(s) helps determine whether specific foods or ingredients in foods contribute to unwanted symptoms. Elimination diets are individualized based on each patient’s history, eating patterns, and overall symptom picture.
What is an elimination diet?
Elimination diets are commonly used tools in functional medicine. The food we eat is the foundation of our wellness yet, some foods, even seemingly healthy ones, may triggers unwanted symptoms in some people. It is estimated that between 2–20% of people worldwide may suffer from some form of a food intolerance. An elimination diet is the process of removing a food or group of foods from a person’s diet for a set period of time. The absence of the food(s) and then careful reintroduction of the item(s) helps determine whether specific foods or ingredients in foods contribute to unwanted symptoms. Elimination diets are individualized based on each patient’s history, eating patterns, and overall symptom picture.
Why complete an elimination diet?
Food sensitivities can be responsible for a variety of symptoms. You may benefit from completing an elimination diet if you struggled with any of the following symptoms:
Bloating
Heartburn
Distention
Constipation
Diarrhea
Fatigue
Difficulty sleeping
Skin rashes
Headaches
Low mood
Common types of elimination diets:
FODMAP Diet: This diet eliminates foods high in certain carbohydrates (Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols) that can be difficult to digest and may cause digestive symptoms such as bloating, gas, and diarrhea. It is often used to manage irritable bowel syndrome (IBS) or other functional gastrointestinal disorders.
Gluten-Free Diet: This diet eliminates all sources of gluten, a protein found in wheat, barley, rye, and some other grains. It is necessary for individuals with celiac disease, an autoimmune disorder triggered by gluten, and may also be followed by those with non-celiac gluten sensitivity.
Dairy-Free Diet: This diet eliminates all dairy products, including milk, cheese, yogurt, and butter. It is commonly followed by individuals with lactose intolerance, a condition in which the body has difficulty digesting lactose, the sugar found in dairy products. It may also be followed by individuals with milk protein allergies.
Specific Carbohydrate Diet (SCD): This diet eliminates complex carbohydrates, disaccharides, and certain grains. It is often used to manage digestive disorders such as Crohn's disease, ulcerative colitis, and celiac disease.
Low-Histamine Diet: This diet restricts foods that are high in histamine or release histamine in the body. It is followed by individuals with histamine intolerance, a condition characterized by an inability to properly break down histamine, leading to symptoms such as headaches, flushing, hives, nasal congestion and digestive issues.
Whole30: Whole30 is a 30-day elimination diet that removes grains, legumes, dairy, added sugars, processed foods, and certain food additives. It is designed to reset eating habits, identify food sensitivities, and promote overall health and well-being. It is not specifically designed for a particular health condition.
Autoimmune Protocol (AIP) Diet: The AIP diet eliminates foods that may trigger inflammation and exacerbate autoimmune conditions. It eliminates grains, legumes, dairy, eggs, nightshade vegetables, nuts, seeds, refined sugars, and processed foods. The AIP diet is often recommended for individuals with autoimmune diseases who are looking to manage their symptoms and reduce inflammation. It eliminates potential trigger foods to support immune system regulation.
Six Food Elimination Diet: This diet is often used in the diagnosis of food allergies in children. It helps identify specific allergenic foods that may be causing symptoms such as skin rashes, digestive issues, or respiratory problems. It eliminates the most common allergenic foods, including milk, eggs, peanuts/tree nuts, soy, and wheat.
These are just a few examples of elimination diets, and there may be variations or combinations of these diets based on individual needs and specific health conditions. It's important to consult with a healthcare professional or registered dietitian before starting an elimination diet to ensure proper guidance and monitoring throughout the process.
What to expect on an elimination diet:
Duration of the Diet: During the elimination phase, you will remove certain foods from your diet based on the specific type of elimination diet you are following. This phase typically lasts for a few weeks to several months, depending on the diet and your individual needs.
Potential Withdrawal Symptoms: Some people may experience withdrawal symptoms when cutting out certain foods, particularly those containing caffeine or sugar. These symptoms can include headaches, irritability, and fatigue. These effects should subside after a few days as your body adjusts.
Improved Symptoms: If you have food sensitivities or intolerances, you may notice a reduction in symptoms during the elimination phase. For example, digestive issues, skin problems, or respiratory symptoms may improve as you remove trigger foods.
Food Reintroduction: After the elimination phase, you will start reintroducing the eliminated foods one at a time in a systematic manner. This is usually done over several weeks, and each food is reintroduced individually, allowing you to observe any reactions.
Identification of Food Sensitivities: The primary goal of an elimination diet is to identify any food sensitivities or intolerances. By reintroducing foods one by one, you can pinpoint which ones are causing adverse reactions.
Increased Awareness of Eating Habits: Elimination diets often require careful reading of food labels and increased awareness of ingredients. This can lead to improved knowledge about the foods you consume and better eating habits.
Emotional Challenges: Elimination diets can be challenging, especially if you have to give up favorite foods or make significant dietary changes. This might cause some emotional ups and downs during the process.
Support and Guidance: Having a healthcare professional or registered dietitian guide you through the elimination diet can be highly beneficial. They can help you plan your meals, monitor your progress, and provide support throughout the process.
Reintroduction Reactions: Some individuals may experience reactions when reintroducing certain foods. These reactions could be mild or more severe, depending on the level of sensitivity. If you experience severe reactions, it's essential to stop consuming the food and consult with a healthcare professional.
Is there a blood test to use instead of completing an elimination diet?
There are many lab tests availalve that measure certain antibodies or biomarkers in the blood that are associated with an immune response to specific foods. They claim to identify which foods might be triggering adverse reactions in individuals. However, food sensitivity tests have many challenges including lack of standardization, difficulty interpreting the significance of IgG antibodies and potential cross-reactions between foods. Food sensitivities are complex and can involve various immune mechanisms. Blood tests often oversimplify the process by focusing on just a few markers, potentially missing other important factors.
Due to these limitations, many healthcare professionals and experts still consider elimination diets as the gold standard for identifying food sensitivities or intolerances. Elimination diets allow for a more comprehensive and personalized approach, and they are more likely to provide accurate results in identifying specific trigger foods.
If you are considering food sensitivity testing, it's crucial to consult with a qualified healthcare professional who can help you understand the limitations and implications of the test results. They can also guide you on the most appropriate approach to identifying and managing potential food sensitivities based on your unique health needs and history.
Relish Health offers a Whole30-style, physician-guided elimination diet. The 50-day program guides you through removal of specific foods from your diet for 30 days. This 30-day period is proceeded by 10-days of preparation and followed by 10 days of careful food reintroduction. The course provides step-by-step instructions, meal plans, and resource guides. During the months of January and September, Dr. Leazenby is available to answer questions and provide encouragement through facebook and live zoom classes.